 "My stomach hurts all the time", lamented my third client. That is, my 3rd client today alone. She continued, "I'm bloated all the time, even with healthy food. I'm constipated, then I have loose stool. I never feel like I'm getting everything out!". I also work with her father, who has heartburn, a "noisy gut" and suffers from urgent abdominal pain any time he has to go outside of the house. 2 out of 3 clients I work with have digestive issues. As long as I can remember, I have had abdominal pain while eating dinner. My immediate family all suffer from Irritable Bowel Syndrome ("Ass Crisis", as we've affectionately deemed it). I have had a vested interest in learning and working with the digestive system from the day I saw my first client. Fortunately, I have found that most "gut problems" respond extremely well to Naturopathic medicine. If you, or someone you love, has been suffering, this post is for you. The Digestive System - more than just your stomach The digestive system encompasses everything from your mouth down until you see it in the toilet (hopefully) the next day. The Head Digestion starts in the brain, evoking a physical response long before food passes your lips. When we think about food, envisioning how it will taste and feel and actually let ourselves feel hungry, our body gets to work increasing saliva, stomach acid and digestive enzymes. Like a good seduction, digestion is as much a head game as the act of doing it. Problem Zone 1: eating mindlessly, not letting yourself get hungry, eating in a rush, over-eating etc. so that your body doesn't have time to catch up The Mouth Chewing your food thoroughly accomplishes two things:
Problem Zone 2: eating without thoroughly chewing, drinking large amounts of fluids with meals that may dilute your digestive enzymes The Esophagus The esophagus is a flexible tube that carries food from your mouth to your stomach. At the bottom of the esophagus/top of the stomach is a muscle called the lower esophageal sphincter or the cardiac sphincter. When it opens it allows food from the esophagus in the stomach, otherwise it should stay shut to prevent splash up of acid causing heartburn. Problem Zone 3: eating too quickly so that food gets stuck or the stomach becomes overloaded; heartburn that creates pain in the esophagus The Stomach In the stomach, hydrochloric acid (HCl) is produced by the parietal cells in the stomach. Another enzyme called pepsin begins to work on the food as well, breaking down protein. An acidic environment is required to breakdown our food and prevent pathogens (bacteria, fungi, parasites and other food borne illnesses) from taking hold. After churning in the stomach, the partially digested food (now called chyme) moves past the pyloric sphincter at the base of the stomach and empties into the upper small intestine. Problem Zone 4: inadequate stomach acid causing poor digestion of food, heartburn and increasing risk of illness, ulcers Liver/Gallbladder/Pancreas As food enters the upper portion of the small intestine, it passes nearby to the liver, gallbladder and pancreas, which all make enzymes to help us digest fats, proteins and carbohydrates (lipase, protease, amylase and others like lactase for digesting lactose, renin, sucrase etc.). This will result in further breakdown of our food. Problem Zone 5: inadequate fat in diet to stimulate production of lipase and bile, not enough protein in diet to make these enzymes, blood sugar issues that compromise the pancreas' ability to manufacture amylase and keep blood sugar in check, poor functioning of the liver and gallbladder The Small Intestine The small intestine has three parts: the duodenum, jejenum and ileum and collectively is about 6 meters (20 feet) long in humans. As it passes through each of these, food interacts with the lining of the intestines, is absorbed and utilized by the rest of the body. Nutrients from our food are absorbed along the small intestine and breakdown continues. Problem Zone 6: food sensitivities create inflammation along the lining of the small intestine resulting in poor digestion and impaired absorption of nutrients. These can create very dramatic digestive symptoms, and malnutrition. Colon Issues The mostly digested food enters the large intestine, where water is reabsorbed back into the body along much of its 1.5 meters (5 feet). Different kinds of bacteria work on breaking down the remnants here. Problem Zone 7: poor bacteria in the colon can cause bloating, gas, distention and pain. Rectal Issues Finally, stool exits the body. Stool is mainly water, combined with food remnants, dead bacteria and cellular waste. If there is inflammation here or in the colon, the remaining material may not be broken down properly. Problem Zone 8: Hemorrhoids and anal fissures (small cracks around the anus) can block the passage of stool and create pain, bleeding and tearing of the delicate tissue. Putting It All Together (The Digestive Dream!): Top 10 Tips to Hack YOUR Digestive System:
If you experience gas, bloating, heartburn, diarrhea, constipation or other digestive concerns and are interested in learning more, please schedule your Free 15 Minute Health Discovery Session with me. In health & happy digestion,
0 Comments
 "Dr. K, I'm doing great... except that I want to scratch my eyes out, my nose keeps running and I'm going to start charging that frog in my throat rent!" lamented one of my patients this week. And she isn't alone. Seasonal allergies affect 1 in 25 Canadians, according to the Canadian Allergy, Asthma and Immunology Foundation. Allergic rhinitis, or "hay fever", or these damn allergies can present as watery itchy eyes, runny nose with clear mucous, sinus congestion and pressure, itchy tongue and palate, a dry scratchy throat, feeling fatigued, poor concentration. This means lower productivity at work, an increased risk of asthma and an expensive trip to the pharmacy or health food store trying to find relief. Windsor and Toronto are some of the worse cities in Canada to live in with respect to pollution and ragweed. Here in Stratford, we are surrounded by a lot of farmland and trees, which also translates to pesticides and tree pollen. Despite being convenient for travel, this Highway 401 corridor that I and my patients call home can cause some decided health issues from early spring until late fall. So what's an allergy sufferer to do? 1. Catch the culprit Most seasonal type allergies are IgE-mediated immune reactions. A simple skin or blood test can be ordered by your family doctor or Naturopathic Doctor to determine the cause of your symptoms. Common culprits are tree pollens, ragweed, moulds, and dust mites. These can be made worse by certain foods, particularly food sensitivities. 2. Support your immune system Eat a diet high in fresh fruits and vegetables for lots of Vitamin C, good quality probiotics recommended by your health care provider, fermented foods like kombucha, sauerkraut or kefir, and healthy fats. Minimize sugars, processed foods and alcohol as they will suppress your immune function and can contribute to mucous production. 3. Create a customized plan Your family doctor or allergist might also recommend avoiding the allergen if possible, antihistamines or decongestants. Please be aware that decongestant nasal sprays often cause rebound congestion once you discontinue their use, so these should only be used short-term. In my practice, I recommend an individualized supplement program including homeopathics, and nutraceuticals, dietary support and at-home care. I like to recommend using a neti pot filled with a warm sterile saline solution to rinse out the sinuses twice daily during allergy season. It really works! BONUS I also recommend Allergy Booster "shots" preventatively for patients that predictably experience symptoms at this time of year. A simple, low-cost oral solution that can help to improve our immune function and reduce the severity, this is one of my favorite ways to stay on top of allergies. Many of my patients have experienced a dramatic improvement in their allergy symptoms after only a few doses and no longer need to rely on allergy medication. If you or your loved ones are suffering from seasonal allergies, you can book a free 15 minute health strategy session to learn more about treating your allergies.. naturally. In health, Dr. Keila
Food can be the perfect medicine... or the best poison.Our body does the best it can and can only run off the fuel we give it. While most of us try to eat healthily the majority of the time, sometimes the "good" foods we are regularly recommended can make us feel ill. If we are taking in foods that don't agree with us, regardless of which Food Guide or expert recommends them, our body will mount a reaction in order to tell us that we shouldn't eat it. If we continue to consume these foods, the body turns up the dial until we have to listen. Your Cheat Sheet to Food Reactions:
Timing is everythingOne reason it can be so difficult to identify a food reaction is that we may react hours, days or even weeks after ingesting the food in question. If you tend to eat a highly varied diet or eat the same foods over and over, pin-pointing that one meal can be a challenge, particularly if you started to feel crummy a few days later. Trust your gut..but look for other clues.The gut is the gateway to the rest of the body. If a food reacts in our gut, it impacts not only our digestive function, but the rest of our body as well. In particular, the immune system, neurological and reproductive systems get involved. Symptoms of a food sensitivity can include:
Your symptoms may evolve over time as well. For example, I notice with myself that when I eat gluten I start to feel very sleepy and have an immediate-onset brain fog. If I continue to ignore my body and eat more - I am the first to admit I am very human and not immune to a fresh slice of bread from time to time - I get some pretty intense stomach cramps and constipation. Since I so seldom eat it, I notice this right away. When I was in university on a tight student's budget, I tended to a lot of pasta (it was cheap, quick and filling) I suffered from debilitating sleep attacks plus all those digestive symptoms, weight gain around the middle and acne. Eventually I realized from trial and error that it was worth spending a few extra bucks, saving the gluten/starch binges for a very occasional treat in order to be more productive, focused, energetic and healthy. As you can see, it certainly goes beyond the digestive system! So how do I know if there's a problem... and what can I do about it?If you're asking yourself this, you've come to the right place!
Working with your family doctor or allergist, standard allergy testing is often recommended to test for IgE-type reactions. Treatment then involves taking an antihistamine (Reactine, Benedryl etc.), epinephrine (eg. carrying an Epi-pen) and/or complete avoidance. However, by now you will realize that IgE reactions are just a small part of the picture. Here is how I treat food reactions:
If you or someone you know is suspects that a food reaction might be contributing to feeling unwell, I would like to offer you a complimentary 15 minute consultation with me to discuss your concerns.  http://cdn.vogue.com.au/media/articles/7/2/0/7267-1_n.jpg?150136 http://cdn.vogue.com.au/media/articles/7/2/0/7267-1_n.jpg?150136 Irritable Bowel Syndrome (IBS) affects people of all ages, however females, and young adults are most likely to be diagnosed. Symptoms can range from cramping, bloating, diarrhea, constipation, incomplete voiding, mucous, nausea and heartburn. Canada and other more well-off countries tend to have much higher rates of IBS, representing a major quality of life burden. While many people are told that they have IBS (and that's that), they might not realize that there's more to it than a bathroom crisis. 1. IBS is not a diagnosis, it is a catch-all. In medicine, we call this a diagnosis of exclusion. This means that before IBS is diagnosed, we need to rule out more serious pathology like Ulcerative Colitis, Crohn's Disease, Colorectal Cancer, Celiac Disease and other immune related conditions. If you are suddenly experiencing a change in bowel patterns, including mucous or blood in your stool, have unexplained weight loss, fever and family history of colon cancer, this merits a thorough medical workup. In the absence of these things, IBS is considered a functional disorder, wherein you experience the symptoms (which can sometimes be very severe) but very little can be seen via labwork or exploratory imaging. 2. Irritable bowel syndrome can include constipation, diarrhea or both. The Rome-III Criteria are used to identify most cases of IBS. This includes recurrent abdominal pain or discomfort at least 3 days per month in the last 3 months, associated with 2 or more of the following:
3. You are what you eat - and what you eat matters! Many people with IBS know one or two foods that set them off, and are careful to avoid it. What you may not know is that your body might actually be having a full-on immune reaction to some of the foods you eat on a regular basis - causing the digestive upset and bathroom angst. Food sensitivities are quite common amoungst people with IBS and it is worth doing a trial elimination diet where you remove the typical offending foods such as gluten, dairy, eggs, soy, citrus, and pork for a period of time and then slowly reintroduce them back into your diet. There are tests to help determine which foods your body is reacting to as well - and these can be quite effective and simple to run. Processed foods, particularly those containing a lot of trans fats, sugars, salts and additives like MSG are the culprit for many people. A diet focused on lots of cooked vegetables, good quality lean protein and some healthy fats like coconut oil, ghee and olive oil can help decrease the severity of IBS. Likewise, a history of multiple rounds of antibiotics can predispose towards IBS as your own natural bacteria gets altered. Probiotics containing Lactobacillus can be helpful for increasing the amount and types of good bacteria in the gut and decreasing IBS symptoms. See a Naturopathic Doctor to decide which strains of probiotics are most appropriate for you. 4. Trust your gut Our guts are extremely sensitive to changes in hormones, including stress hormones like cortisol, and adrenaline and those related to mood like serotonin and dopamine. In fact, we also have a nervous system in our gut - the Enteric Nervous System - that also responds to the same chemicals that influence our brain. This means that when we are stressed out, it can definitely affect our digestive system on a molecular level such that we may feel the urge to go to the bathroom, lose our appetite or get unexplained stomach aches. When working with IBS, it is important to address the mind-body connection via stress management, like exercise, deep breathing, meditation as well as perhaps some botanicals and supplements to improve both your mood and belly. If your gut has been compromised by parasites, Candida, mould, bacterial or viral infections you may be more likely to have IBS either temporarily or in the future. A good treatment plan addresses the cause of your IBS and works on healing the gut. 5. Fibre might be the the answer - or your frenemy. People with IBS are often told by their family doctors and dieticians to increase fibre in their diet. The rationale is sound: more fibre = slower bowel transit time = less diarrhea. Fibre can also help to bind excess hormones, lower cholesterol, stabilize blood sugar and feed the good bacteria in the gut. On the other hand, too much fibre without large amounts of water to accompany it can easily sit like a lead weight in your gut and make you feel like you've swallowed a brick. It can also impair your absorption of vitamins and minerals - not to mention prescription medications - as it literally absorbs things around it. For people tending towards constipation, fibre can cause even more difficulty with bowel movements. The type of fibre needs to be considered as well. While wheat bran is readily available, many people are also sensitive to gluten and will feel worse taking it. 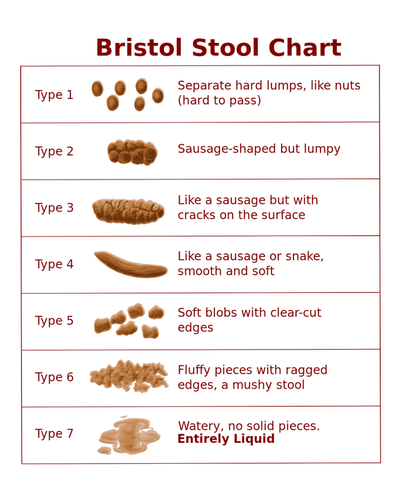 The Bristol Stool Chart is a commonly used visual to help people describe how their bowel movements look to their physicians. Here's the low-down: Type 4 is considered the "perfect poo" - soft, easy to pass, very few/no wiping needed. No cracks, or lumps, even in consistency and color. Type 1-3 equals varying degrees of constipation and dehydration. If we are dehydrated, our body will absorb water wherever it can. Given that our stool is mostly water, you can guess where our body gets some of that liquid. Gross. The longer stool stays in your colon, the more water gets reabsorbed, the drier it gets and more difficulty to pass. Type 5 is typical of people eating a mostly veggie based diet. Type 5-7 points towards malabsorption, food sensitivities or infection. If your stool is loose, runny or very frequent, it is likely that it is passing too quickly through the colon. Dehydration is also a concern as we can lose massive amounts of fluid via diarrhea. Eliminating foods that cause inflammation, treating infections or parasites, adding fibre, proper hydration and some botanicals to slow absorption can be very helpful in these cases. 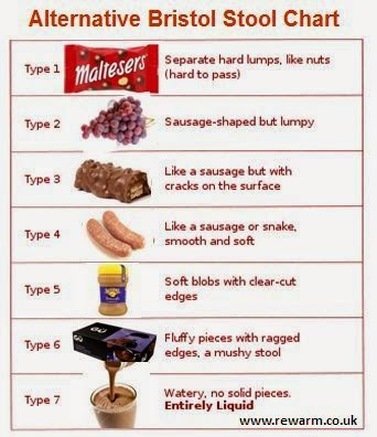 If this looks a little more familiar to you, great, I'm all for everyone being on the same page. We may have also found out why you have IBS since processed foods like these often worsen IBS. If you or someone you know is experiencing Irritable Bowel Syndrome, please book a consultation with me to discuss your options. I have worked with many people experiencing a range of digestive issues using a blend of nutritional medicine, supplements, stress management techniques and acupuncture to help them experience lasting relief.  http://vipmobiledayspa.wordpress.com/2013/06/28/super-foods-that-fight-acne/ http://vipmobiledayspa.wordpress.com/2013/06/28/super-foods-that-fight-acne/ Ugh. 7 am. There's a bright red, angry monster that somehow took up residence on your chin overnight and is now staring back at you in the mirror. The beast hurts when you touch it. It is also probably giving you the stink-eye, just in time for your incredibly important interview. I've been there too. As a teen I had acne so bad it covered my face, chest and back. I went through years of antibiotic creams, washes, birth control pills that I never wanted, and Proactive facial care systems that stained all of my mother's towels. I was even on Accutane for two years. A high dose pharmaceutical variation on Vitamin A, Isotretinoin or Accutane, is commonly prescribed for severe cystic acne. While it is known teratogen (meaning that it is known to cause severe birth defects), a less common side effect of the drug is anxiety, depression and even suicidality. Fun times for me, when both me and my high school boyfriend were taking long courses of Accutane. It worked, however it was a pretty dark time and I'm lucky my family was so patient with me. It has since been taken off the market in Canada due to a possible link between use and Inflammatory Bowel Disease. Yikes! Acne vulgaris (the medical, even uglier sounding term) can be caused by a number of concerns, including: Hormonal imbalances - excess testosterone, or excess estrogen, PCOS, puberty, pregnancy/post-partum, menopause hormonal changes Food sensitivities - dairy, gluten, eggs are the most common although there are many other possible culprits, sugar, preservatives Digestive Weakness - low stomach acidity, excess protein (often from conventionally raised animals whose meat is pro-inflammatory and hormone-laden), poor gut flora, recent antibiotic use Medications - corticosteroids, oral contraceptives, anabolic steroids Allergies - cosmetics, chemicals, fragrances, clothing material, detergent Stress - lack of sleep, stress hormones in overdrive, less-than-scrupulous (or overly vigorous) hygiene But I'm not a teenager anymore! While it can be pretty devastating dealing with acne as a teen, most of us grow out of it. However, some people have acne lasting well into their 30's and 40's. Many others are suddenly faced with some angry crops of acne as adults. Several women I see with adult acne struggle to be taken seriously in their professional lives while feeling that that they look like a kid. Acne is not uncommon in the body-building world either, as anabolic steroids, sweaty work-out cloths and high amounts of whey protein powders can contribute to facial and b-acne. In these cases, look to food sensitivities and other environmental factors. Another form of adult acne, Rosaceae, is often related to low stomach acid or or food sensitivities. So what can I do for my adult acne? 1. Ditch the chemical laden products - Check out EWG's Skin Deep Cosmetic Database to determine if your cosmetics and personal care products could be contributing to your symptoms. Pay particular to expensive high-end brands - many of them have some particularly nasty ingredients. 2. Switch to raw honey as a facial cleanser. Full of good bacteria, honey acts as a skin normalizer for both oily and dry skin and promotes healing. 3. a) Limit sugar, dairy and processed foods. Low glycemic diet and acne (American Journal of Clinical Nutrition, 2007), Acne: the role of medical nutrition therapy (Journal of the Academy of Nutrition and Dietetics, 2013) b) Clean up your diet. Focus on lots of orange and yellow fruits and vegetables like carrots, winter squash, and pumpkin as they contain beta-carotene to help improve skin health. Leafy greens such as dandelion, beet greens, spinach, kale, chard, water cress, blue-green algae (spirulina, seaweeds) tonify the liver to help balance hormones. Mung beans, adzuki beans, unpeeled cucumber slices, alfalfa and soy sprouts are all used in Traditional Chinese Medicine for the treatment of acne as well. 4. Drink lots of water and green tea. Your kidneys and liver filter toxins out of your body - staying well hydrated assists this function. 5. Adopt a regular stress management practice. Acne is associated with lower self-esteem, higher and rates of depression - Understanding the burden of adult female acne (Journal of Aesthetic and Clinical Dermatology, 2014). Yoga, deep breathing, and exercise can be helpful for confidence breathing, handling stress and improving your quality of life. Check out Jean's story... this is a great example of how naturopathic medicine can help treat adult acne with amazing results! Naturopathic approaches to acne involve removing food sensitivities, creating a tailored supplement protocol, stress management exercises and hormonal support as needed to help resolve current acne, minimize scarring and reduce the occurrence of future outbreaks. If you are struggling with acne - whether you are a teen or a grandmother or anywhere in between - let's set up a time to chat. Here's to your clear skin! Dr. Keila |
Top 75 Naturopath Blogs & Websites For Naturopathic DoctorsAuthorDr. Keila Roesner is a Naturopathic Doctor. When not treating patients she is also an enthusiastic barefoot-strolling, music-loving, yoga-doing kitchen wiz - who also happens to be a wrestling fan. Categories
All
|
Let us take you from hormonal to whole.
|
Dr. Keila Roesner, BHSc ND
Naturopathic Doctor, Hormone Warrior and Your Wellness Cheerleader 247 Church Street, Stratford ON N5A 2R7 (519) 273-0900 drkeila@roesnerwellnesssolutions.com |
|




 RSS Feed
RSS Feed