|
Irritable Bowel Syndrome was traditionally a "diagnosis of exclusion" and often considered if a colonoscopy (checks the colon) and endoscopy (checks the esophagus and stomach) look normal. Basically this means that your physician has hopefully ruled out the scary things like Crohn's disease, ulcerative colitis, and colon cancer and while your digestive system is a mess, you are "normal and healthy".
Time to call B.S. Irritable Bowel Syndrome: constipation, diarrhea, urgent runs to the bathroom, 3 months pregnant food baby bloating, gas and pain are anything BUT normal. In our previous posts we have discussed some of the most common causes of IBS and some basics to help get you feeling better. Personally, I believe that the more information we have, the better you will do. With that information you can create a logical plan to feel better. When you feel better you can work more effectively, spend better quality time with your family and spend less time feeling awful. While every person is different, here are the 6 most common tests I recommend anyone with Irritable Bowel Syndrome consider: The Basics:
Specialized Tests:
When you are armed with the right information you can stop wasting time running between doctor's visits, trying expensive supplements that don't work and medications that create other nasty side effects. With the right information you can start feeling better. If you are ready to start feeling better, please contact me to book your complimentary Health Discovery Session. In health,
0 Comments
 What if Irritable Bowel Syndrome (IBS) wasn't "just in your head?". This may seem revolutionary for many physicians... and people that don't have IBS. Anyone living with IBS knows it's true. Nobody wants to be bathroom bound when they try to leave the house, or have to scan a restaurant menu frantically looking for the one item that won't cause them pain or embarrassing gas within an hour. Well, it's true. Small Intestinal Bowel Overgrowth (SIBO) is estimated to be the cause of anywhere from 40-85% or more cases of IBS. Clinically, I would say that this number is even higher. Your Gut is a Garden There are several types of bacteria within the digestive system. The particular species depend on things like your genetics, your birth type (hospital, home birth, vaginal, C-section), breast versus formula feeding, your diet, medications and stress. They can change over time and the unique combination can markedly affect how you feel. It can be helpful to classify human bacteria into three categories:
Much like a garden, there are a combination of plants that you want like tomatoes, sunflowers, parsley (healthy bacteria), species that show up that can take over if not contained like mint, orange lilies (commensals) and then there are invasive weeds like bindweed, thistles (pathogenic bacteria). Every garden will have a combination of all of these. As in the human digestive system, we want the balance to be tipped in favour of the helpful species, so that the neutral species can exist in manageable amounts, and hopefully ultimately crowd out the weeds. A diligent gardener can also go a long way. Normally, the majority of bacteria within the digestive system reside within the large intestine where they work on the food you're digesting to produce Vitamins B1, B2, B6, B12 and K2 as well as other substances. Since we have 10 times as many bacterial cells in our body as we have human cells, even a small alteration in our bacterial garden can change our landscapes dramatically. Our In House Gardener: The Migrating Motor Complex (MMC) The MMC coordinates electrical wave patterns every 90-120 between meals that sweeps through the stomach and small intestine to helps propel food and bacteria from the ileum (the end segment of the small intestine) to the large intestine. In order to function properly, our body needs to have a break between meals. In SIBO, these bacteria can migrate backwards, up into the small intestine which normally has far fewer bacteria. This migration can occur with intestinal permeability, certain medications, inflammatory bowel disease (Ulcerative Colitis, Crohn's Disease), Celiac disease, and low stomach acid. Because competition is less fierce in the small intestine than in the large intestine [Read my previous blog here to review], these bacteria can settle in, replicate and grow without being crowded. This is like freshly tilling your garden and then going on vacation for two weeks only to find that your neighbour's weeds crept under the fence and have taken over. Now you have thistles that are six feet tall. The problem is that now you have bacteria existing in high amounts where they would not normally be and they are now crowding out healthy bacteria, interfering with your crop and attracting pests. The overgrowth can be a combination of healthy, commensal or pathogenic bacteria.... it doesn't really matter because you've got a forest on your hands. This overgrowth is what contributes to much of the discomfort of Irritable Bowel Syndrome. Have you ever noticed that flowers are easily pulled but weeds have deep roots? Same story here. The bacteria that takes hold likes to stick around and make a mess. It can throw off the MMC, and instead of helping to digest your food it ferments it. Fermentation is the process of converting sugars in foods to gases or alcohol, as in beer, wine and sourdough bread. Our bodies are not designed to ferment, and when we do, we bloat. We get gas pains and "I swear I'm not 3 months pregnant!" food babies after eating. Because the food is not breaking down properly, we also get intestinal permeability. We are more likely to have other problems too:
Sound familiar? In our next blog post, we are going to be covering the key signs to watch out for to tell if you have SIBO and what you can do about it. If you found this post helpful, please share with your friends and family! In happy digestive health, Dr. Keila
References
 I had a potential new client in my office today who had been diagnosed by her family doctor with Irritable Bowel Syndrome several years ago. When she asked what she should do next, he told her to "go read about it". Wait, what?! There is so much misinformation online: treatments based on outdated science, "it-worked-for-my-sister's-neighbour" stories and down right bad advice. Unfortunately, she did not have a medical degree or background in research to be able to decipher the good from the bad. She knew that the info she was seeing on Yahoo forums was probably questionable, she didn't know where to go to find good information. So she was referred by her pelvic floor physiotherapist to me. "Reading about it" had done nothing for her and she was sick and tired of daily diarrhea. She is not alone. One of the most common causes of IBS is a little known condition called Small Intestinal Bacterial Overgrowth (SIBO) - [read my previous blog post here]. While you should absolutely work with a knowledgeable health professional, there are several tell tale signs that your IBS is actually due to SIBO (and not a deficiency in "reading about it"). 5 Key Signs You Might Have SIBO:
If any of these sound familiar, let's set up a time to chat. Book your complimentary Health Discovery Session to discuss your options. Getting the right testing is the first step to getting better. The good news is that there are some very good tests you can do to see if SIBO is causing your IBS. Based on your results, we can create a customized plan to get rid of the discomfort, gas, bloating and bathroom embarrassment. Once and for all. In my next blog, we will talk about some of the testing you should have to finally get rid of your Irritable Bowel Syndrome. In health,  Ever had a "Bridesmaid moment"? One of my patients the other day told me about hers. The thing is, she eats exceptionally healthy, exercises, meditates daily and has one of the sunniest outlooks on life I've ever seen. She did not have food poisoning. But her digestive system was a mess. In fact, she had been diagnosed with Irritable Bowel Syndrome (IBS) and her doctor also suspected Irritable Bowel Syndrome is estimated to affect between 10-15% of Canadians (1). I would tend to say that these numbers are extremely conservative because many people with digestive disorders may not seek care from their medical doctors, or it may take several years to receive a diagnosis. In fact, the vast majority of my clients have one or more digestive concerns. If you have one digestive issue you are likely to have another. They are not unrelated. This is not a fluke. And you're not going to fix it unless you treat the whole system, or more practically, treat you as a person rather than a collection of mouths, stomachs, guts and colons. The most common digestive issues that I see and treat are:
Treatment for these concerns may not be particularly helpful and can often cause additional concerns. For example, Proton Pump Inhibitors (PPI) are commonly prescribed to treat heartburn. Side effects of Nexium (Esomeprazole) a common PPI, include constipation, watery diarrhea, abdominal cramps, stomach pain, and nausea (2). Other PPIs may decrease absorption of calcium, magnesium, zinc, iron and vitamin B12, increase risk of Community Acquired Pneumonia, C. difficile infection, Traveler's Diarrhea, and Small Intestinal Bacterial Overgrowth (3). Moreover, these medications work by decreasing acid production within the stomach. While this may alleviate heartburn (read my thoughts on this here), this is like cutting off your nose to spite your face. The thing is, we need lots of stomach acid. The stomach's job is to burn off parasites, molds, bacteria and viruses to help protect our body from infections. Without a strong acid barrier, our body is not going to be able to protect against these nasty things. In particular, heartburn is associated with Small Intestinal Bowel Overgrowth (SIBO) - a condition of inappropriate types of bacteria hanging out in the small intestine where they shouldn't be. This is relevant because SIBO is conservatively estimated to be the direct cause of Irritable Bowel Syndrome in 40-85% of cases. That's right, IBS is not idiopathic or in your head. To add more fuel to the fire, a 2009 study showed that people with GERD were 3.5 x more likely to develop IBS and that people with IBS were 2.8x more likely to develop GERD (4). So, what can we do about it? Treat the Cause. Here are the big priorities.
If you find this article helpful or surprising and would like to learn more, I would love to invite you to book a complimentary Health Discovery Session with me to discuss your options. In happy digestive health, Dr. Keila
References:
 There's a burning fiery pit in your chest. It's not a heart attack. You've checked with your doctor before. It's feels heavy, uncomfortable and burns. At your last visit you were told that you probable have GERD. And you think, "what a goofy name for something that feels like hell!" Heartburn, or Gastroesophageal Reflux Disease (GERD) accounts for one out of three primary care visits, and has been increasing quite dramatically over the last two decades (1). It's now estimated that 18-27% of adults in North America experience heartburn at least once weekly (2), and many experience it daily. Which absolutely sucks. This sharp increase can be attributed to rising rates of obesity, and is more common amoungst smokers and with age. Common symptoms of GERD include:
A diagnosis of GERD is often made at the physicians office, and then commonly, anatacids (Gavison, Rolaids, Tums), H-2 receptor blockers (Pepcid AC, Zantac) or Proton pump inhibitors (PPIs, like Prevacid, Losec etc.) are recommended to "stop the burning". If it helps, it is assumed that GERD was your problem. But we seem to have gotten a little caught up with this idea that burning = too much acid. If you've read my blog "Why Does My Stomach Hurt?" you'll see that it is a little more complicated than that. Heartburn typically stems from one of four causes:
Very rarely have I ever seen increased stomach acid cause heartburn. Rather, it is most likely a combination of low stomach acid, over-eating and a weak lower esophageal sphincter. Zollinger-Eillison Syndrome is the only known cause of increased stomach acid, and is a very rare condition where one or more tumours in the small intestine or pancreas (gastrinomas) secrete a large amount of the hormone gastrin which then causes the stomach to produce too much acid (5). In summary, your stomach is probably not too acidic. But something else is going on, making your uncomfortable. Don't you want to find out.. and fix it? If you or someone you love is experiencing heartburn and want to treat the cause, please book a Free 15 Minute Health Discovery Session with me. In our next few blogs, I will outline how to know if GERD is part of a larger puzzle and how you can start improving it naturally. Until then, happy digesting! References:
 Stopped up. Bunged up. Full of it. Constipated. No fun. Constipation is something I frequently see in practice, and something I notice that tends to effect women, the elderly and people taking more medication more commonly. Increasingly, I am seeing more issues with young women in their teens and twenties. Typical recommendations are to avoid constipation is to increase water and fibre, and to consume more leafy greens (again, more fibre). But what if these things aren't helping... or are making the sh*tty situation worse? Before we get into the why and more importantly, what you can do about it, let's back it up (get it?). You will definitely want to check out my digestion post for more in depth specifics on how the digestive system works. Constipation is defined as infrequent bowel movements that are often difficult to pass and that is lasting a few weeks or more. Many physicians consider constipation to be 3 or less bowel movements per week. On the other hand, Traditional Chinese Medicine and Ayurvedic medicine consider normal frequency to be 1-3 bowel movements per day with any more or less to be abnormal. Normal bowel movements should be easy to pass, solid, medium brown in color, with no undigested bits of food, no blood, no mucous, no straining and with only minimal wiping required. Checking your stool every day is a great way to keep tabs on how things are moving. Constipation can usually be resolved by:
Constipation can also signify:
If you are experiencing frequent or long term constipation, be sure to check with your doctor or Naturopathic Doctor or pelvic floor physiotherapist to rule out the conditions listed above. You can also book a Free 15 Minute Health Discovery Session with me to learn about your options. In health & smooth moves,  "My stomach hurts all the time", lamented my third client. That is, my 3rd client today alone. She continued, "I'm bloated all the time, even with healthy food. I'm constipated, then I have loose stool. I never feel like I'm getting everything out!". I also work with her father, who has heartburn, a "noisy gut" and suffers from urgent abdominal pain any time he has to go outside of the house. 2 out of 3 clients I work with have digestive issues. As long as I can remember, I have had abdominal pain while eating dinner. My immediate family all suffer from Irritable Bowel Syndrome ("Ass Crisis", as we've affectionately deemed it). I have had a vested interest in learning and working with the digestive system from the day I saw my first client. Fortunately, I have found that most "gut problems" respond extremely well to Naturopathic medicine. If you, or someone you love, has been suffering, this post is for you. The Digestive System - more than just your stomach The digestive system encompasses everything from your mouth down until you see it in the toilet (hopefully) the next day. The Head Digestion starts in the brain, evoking a physical response long before food passes your lips. When we think about food, envisioning how it will taste and feel and actually let ourselves feel hungry, our body gets to work increasing saliva, stomach acid and digestive enzymes. Like a good seduction, digestion is as much a head game as the act of doing it. Problem Zone 1: eating mindlessly, not letting yourself get hungry, eating in a rush, over-eating etc. so that your body doesn't have time to catch up The Mouth Chewing your food thoroughly accomplishes two things:
Problem Zone 2: eating without thoroughly chewing, drinking large amounts of fluids with meals that may dilute your digestive enzymes The Esophagus The esophagus is a flexible tube that carries food from your mouth to your stomach. At the bottom of the esophagus/top of the stomach is a muscle called the lower esophageal sphincter or the cardiac sphincter. When it opens it allows food from the esophagus in the stomach, otherwise it should stay shut to prevent splash up of acid causing heartburn. Problem Zone 3: eating too quickly so that food gets stuck or the stomach becomes overloaded; heartburn that creates pain in the esophagus The Stomach In the stomach, hydrochloric acid (HCl) is produced by the parietal cells in the stomach. Another enzyme called pepsin begins to work on the food as well, breaking down protein. An acidic environment is required to breakdown our food and prevent pathogens (bacteria, fungi, parasites and other food borne illnesses) from taking hold. After churning in the stomach, the partially digested food (now called chyme) moves past the pyloric sphincter at the base of the stomach and empties into the upper small intestine. Problem Zone 4: inadequate stomach acid causing poor digestion of food, heartburn and increasing risk of illness, ulcers Liver/Gallbladder/Pancreas As food enters the upper portion of the small intestine, it passes nearby to the liver, gallbladder and pancreas, which all make enzymes to help us digest fats, proteins and carbohydrates (lipase, protease, amylase and others like lactase for digesting lactose, renin, sucrase etc.). This will result in further breakdown of our food. Problem Zone 5: inadequate fat in diet to stimulate production of lipase and bile, not enough protein in diet to make these enzymes, blood sugar issues that compromise the pancreas' ability to manufacture amylase and keep blood sugar in check, poor functioning of the liver and gallbladder The Small Intestine The small intestine has three parts: the duodenum, jejenum and ileum and collectively is about 6 meters (20 feet) long in humans. As it passes through each of these, food interacts with the lining of the intestines, is absorbed and utilized by the rest of the body. Nutrients from our food are absorbed along the small intestine and breakdown continues. Problem Zone 6: food sensitivities create inflammation along the lining of the small intestine resulting in poor digestion and impaired absorption of nutrients. These can create very dramatic digestive symptoms, and malnutrition. Colon Issues The mostly digested food enters the large intestine, where water is reabsorbed back into the body along much of its 1.5 meters (5 feet). Different kinds of bacteria work on breaking down the remnants here. Problem Zone 7: poor bacteria in the colon can cause bloating, gas, distention and pain. Rectal Issues Finally, stool exits the body. Stool is mainly water, combined with food remnants, dead bacteria and cellular waste. If there is inflammation here or in the colon, the remaining material may not be broken down properly. Problem Zone 8: Hemorrhoids and anal fissures (small cracks around the anus) can block the passage of stool and create pain, bleeding and tearing of the delicate tissue. Putting It All Together (The Digestive Dream!): Top 10 Tips to Hack YOUR Digestive System:
If you experience gas, bloating, heartburn, diarrhea, constipation or other digestive concerns and are interested in learning more, please schedule your Free 15 Minute Health Discovery Session with me. In health & happy digestion,  My cat, hiding from me. My cat, hiding from me. I got home at 6:30pm, after a long day of work. Angry. Hungry angry. Hangry. Even my cat was avoiding me. I went straight to the peanut butter jar, dug out the chocolate chips and went to town with my favorite sugar + fat snack. There was no way I could wait to make dinner. I needed a fix. It's hard to be graceful eating peanut butter out of the jar. I'm human, I fully admit it. My eating habits had a long way to go when I first started University, starry-eyed and bound for medical school. Over the first two years, I gained 15 lbs, started losing handfuls of hair, got easily overwhelmed and developed terrible sleeping habits. It was a rough go. By the time I started my Naturopathic medical training at the Canadian College of Naturopathic Medicine I had started making some very significant changes to diet. The biggest changes were cutting out processed crap (like the yellow powdered chicken broth that was previously a staple in my cooking), limiting wheat and increasing fat in my diet. Two years ago, however, I really hit the nail on the head. A colleague of mine, Dr. Erica Robinson, had been a big proponent of the Paleolithic Diet for quite sometime and it got me thinking. The Paleo Diet The Paleolithic Diet is based whole foods - lot of vegetables, a modest amount of fruit, lots of healthy fats and high quality protein - and is meant to simulate the way our ancient human ancestors during the Paleolithic era might have ate. At the same time, this style of eating limits ALL grains, beans and legumes, dairy, sugars, processed foods and alcohol. I know, it does sound drastic at first. Why would you do this to yourself??? We, as a species, have evolved over several hundred thousand years eating a certain way - foraging lots of greens, fruits, edible tubers, nuts and seeds, and when we could find it, meat including the higher fat organ meats. We moved a lot more, slept when the sun went down and had a heck of a lot more downtime to rest and play than we do today. It wasn't until the Neolithic era when agriculture really caught on that we started to settle down and dramatically increased the amount of grains and legumes in our diet. We stayed in one place, had a steady diet of grains, legumes and beans in addition to what those ancient ancestors ate. We had food security. Yes, that did happen thousands of years ago, however even that amount of time is only a small blip compared to the many years of eating in the hunter-gatherer style. The argument is that we are genetically evolved to be eating in this ancient, Paleolithic style, and our genetics are still playing a losing game of catch-up to our agriculture loving ancestor's grain and bean-based diet. Our DNA has no hope in hell to catch up with our modern diet full of genetically engineered wheat, corn, soy, processed fats, sodium, alcohol, antibiotic-laden dairy and other "food products". The Standard American Diet (SAD, for short) is forcing us to fight a bloody, uphill battle against our genetics... and it is one that we can't win. Numerous scientific studies have detailed that the SAD diet full of convenience but absolutely lacking nourishment are direct contributors to heart disease, diabetes, strokes, obesity and cancers amoung MANY other concerns. Yep, these are our biggest killers and we keep getting sicker, fatter, tired, depressed and miserable. So what did this peanut butter-loving Naturopath (to be) do? I read a LOT of books, including these: The Primal Blueprint: Reprogram Your Genes for Effortless Weight Loss, Vibrant Health, and Boundless Energy by Mark Sisson Paleoista: Gain Energy, Get Lean, and Feel Fabulous With the Diet You Were Born to Eat by Nell Stephenson The Paleo Solution: The Original Human Diet by Robb Wolf Practical Paleo by Diane Sanfilippo Make It Paleo: Over 200 Grain Free Recipes for Any Occasion - Bill Staley and Hayley Mason Well Fed: Paleo Recipes for People Who Love to Eat by Melissa Joulwan Dr. Loren Cordain's work and these blogs: Mark's Daily Apple NomNomPaleo Paleo OMG The Clothes Make the Girl I got rid of the grains, the sugar, beans, cut out dairy and threw out anything my great-great-great (x50) grandmother would not recognize as food. I increased the amount of produce I ate, set a limit of max 2 servings of fruit, dramatically increased the healthy fats, had high quality protein with each meal and got to work cooking. I seriously upped the quality of nutrition in my already "healthy" diet. I began to walk everywhere, made yoga a part of my day and allowed myself time to relax. I lost the 15 pounds of stress fat I put on through university and med school. I completely cured my insomnia. My acne cleared. My periods got more regular. I stopped losing handfuls of hair. I got used to saying "No thank you" to well-meaning friends and relatives offering me foods that made me feel ill. I felt truly empowered, knowing that I choose to take my health in my hands every day, that there are answers and that feeling ill did not have to be a given. And I was a heck of a lot more pleasant to be around. Are you interested? Book your free health consultation with me to start living the healthy life you know you deserve. “The food you eat can be either the safest and most powerful form of medicine or the slowest form of poison.” - Anne Wigmore Anne, you are right. I choose medicine. Awesome, tasty medicine. Check out how we do it! - Dr. Keila (no makeup Sunday) Xo
Food can be the perfect medicine... or the best poison.Our body does the best it can and can only run off the fuel we give it. While most of us try to eat healthily the majority of the time, sometimes the "good" foods we are regularly recommended can make us feel ill. If we are taking in foods that don't agree with us, regardless of which Food Guide or expert recommends them, our body will mount a reaction in order to tell us that we shouldn't eat it. If we continue to consume these foods, the body turns up the dial until we have to listen. Your Cheat Sheet to Food Reactions:
Timing is everythingOne reason it can be so difficult to identify a food reaction is that we may react hours, days or even weeks after ingesting the food in question. If you tend to eat a highly varied diet or eat the same foods over and over, pin-pointing that one meal can be a challenge, particularly if you started to feel crummy a few days later. Trust your gut..but look for other clues.The gut is the gateway to the rest of the body. If a food reacts in our gut, it impacts not only our digestive function, but the rest of our body as well. In particular, the immune system, neurological and reproductive systems get involved. Symptoms of a food sensitivity can include:
Your symptoms may evolve over time as well. For example, I notice with myself that when I eat gluten I start to feel very sleepy and have an immediate-onset brain fog. If I continue to ignore my body and eat more - I am the first to admit I am very human and not immune to a fresh slice of bread from time to time - I get some pretty intense stomach cramps and constipation. Since I so seldom eat it, I notice this right away. When I was in university on a tight student's budget, I tended to a lot of pasta (it was cheap, quick and filling) I suffered from debilitating sleep attacks plus all those digestive symptoms, weight gain around the middle and acne. Eventually I realized from trial and error that it was worth spending a few extra bucks, saving the gluten/starch binges for a very occasional treat in order to be more productive, focused, energetic and healthy. As you can see, it certainly goes beyond the digestive system! So how do I know if there's a problem... and what can I do about it?If you're asking yourself this, you've come to the right place!
Working with your family doctor or allergist, standard allergy testing is often recommended to test for IgE-type reactions. Treatment then involves taking an antihistamine (Reactine, Benedryl etc.), epinephrine (eg. carrying an Epi-pen) and/or complete avoidance. However, by now you will realize that IgE reactions are just a small part of the picture. Here is how I treat food reactions:
If you or someone you know is suspects that a food reaction might be contributing to feeling unwell, I would like to offer you a complimentary 15 minute consultation with me to discuss your concerns.  http://cdn.vogue.com.au/media/articles/7/2/0/7267-1_n.jpg?150136 http://cdn.vogue.com.au/media/articles/7/2/0/7267-1_n.jpg?150136 Irritable Bowel Syndrome (IBS) affects people of all ages, however females, and young adults are most likely to be diagnosed. Symptoms can range from cramping, bloating, diarrhea, constipation, incomplete voiding, mucous, nausea and heartburn. Canada and other more well-off countries tend to have much higher rates of IBS, representing a major quality of life burden. While many people are told that they have IBS (and that's that), they might not realize that there's more to it than a bathroom crisis. 1. IBS is not a diagnosis, it is a catch-all. In medicine, we call this a diagnosis of exclusion. This means that before IBS is diagnosed, we need to rule out more serious pathology like Ulcerative Colitis, Crohn's Disease, Colorectal Cancer, Celiac Disease and other immune related conditions. If you are suddenly experiencing a change in bowel patterns, including mucous or blood in your stool, have unexplained weight loss, fever and family history of colon cancer, this merits a thorough medical workup. In the absence of these things, IBS is considered a functional disorder, wherein you experience the symptoms (which can sometimes be very severe) but very little can be seen via labwork or exploratory imaging. 2. Irritable bowel syndrome can include constipation, diarrhea or both. The Rome-III Criteria are used to identify most cases of IBS. This includes recurrent abdominal pain or discomfort at least 3 days per month in the last 3 months, associated with 2 or more of the following:
3. You are what you eat - and what you eat matters! Many people with IBS know one or two foods that set them off, and are careful to avoid it. What you may not know is that your body might actually be having a full-on immune reaction to some of the foods you eat on a regular basis - causing the digestive upset and bathroom angst. Food sensitivities are quite common amoungst people with IBS and it is worth doing a trial elimination diet where you remove the typical offending foods such as gluten, dairy, eggs, soy, citrus, and pork for a period of time and then slowly reintroduce them back into your diet. There are tests to help determine which foods your body is reacting to as well - and these can be quite effective and simple to run. Processed foods, particularly those containing a lot of trans fats, sugars, salts and additives like MSG are the culprit for many people. A diet focused on lots of cooked vegetables, good quality lean protein and some healthy fats like coconut oil, ghee and olive oil can help decrease the severity of IBS. Likewise, a history of multiple rounds of antibiotics can predispose towards IBS as your own natural bacteria gets altered. Probiotics containing Lactobacillus can be helpful for increasing the amount and types of good bacteria in the gut and decreasing IBS symptoms. See a Naturopathic Doctor to decide which strains of probiotics are most appropriate for you. 4. Trust your gut Our guts are extremely sensitive to changes in hormones, including stress hormones like cortisol, and adrenaline and those related to mood like serotonin and dopamine. In fact, we also have a nervous system in our gut - the Enteric Nervous System - that also responds to the same chemicals that influence our brain. This means that when we are stressed out, it can definitely affect our digestive system on a molecular level such that we may feel the urge to go to the bathroom, lose our appetite or get unexplained stomach aches. When working with IBS, it is important to address the mind-body connection via stress management, like exercise, deep breathing, meditation as well as perhaps some botanicals and supplements to improve both your mood and belly. If your gut has been compromised by parasites, Candida, mould, bacterial or viral infections you may be more likely to have IBS either temporarily or in the future. A good treatment plan addresses the cause of your IBS and works on healing the gut. 5. Fibre might be the the answer - or your frenemy. People with IBS are often told by their family doctors and dieticians to increase fibre in their diet. The rationale is sound: more fibre = slower bowel transit time = less diarrhea. Fibre can also help to bind excess hormones, lower cholesterol, stabilize blood sugar and feed the good bacteria in the gut. On the other hand, too much fibre without large amounts of water to accompany it can easily sit like a lead weight in your gut and make you feel like you've swallowed a brick. It can also impair your absorption of vitamins and minerals - not to mention prescription medications - as it literally absorbs things around it. For people tending towards constipation, fibre can cause even more difficulty with bowel movements. The type of fibre needs to be considered as well. While wheat bran is readily available, many people are also sensitive to gluten and will feel worse taking it. 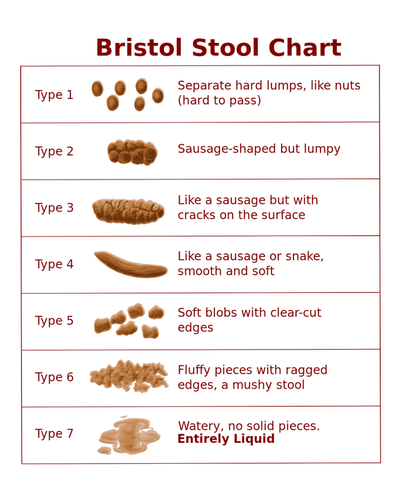 The Bristol Stool Chart is a commonly used visual to help people describe how their bowel movements look to their physicians. Here's the low-down: Type 4 is considered the "perfect poo" - soft, easy to pass, very few/no wiping needed. No cracks, or lumps, even in consistency and color. Type 1-3 equals varying degrees of constipation and dehydration. If we are dehydrated, our body will absorb water wherever it can. Given that our stool is mostly water, you can guess where our body gets some of that liquid. Gross. The longer stool stays in your colon, the more water gets reabsorbed, the drier it gets and more difficulty to pass. Type 5 is typical of people eating a mostly veggie based diet. Type 5-7 points towards malabsorption, food sensitivities or infection. If your stool is loose, runny or very frequent, it is likely that it is passing too quickly through the colon. Dehydration is also a concern as we can lose massive amounts of fluid via diarrhea. Eliminating foods that cause inflammation, treating infections or parasites, adding fibre, proper hydration and some botanicals to slow absorption can be very helpful in these cases. 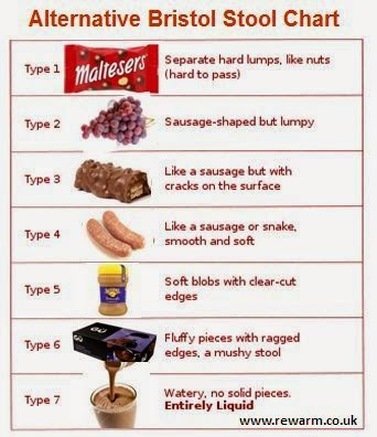 If this looks a little more familiar to you, great, I'm all for everyone being on the same page. We may have also found out why you have IBS since processed foods like these often worsen IBS. If you or someone you know is experiencing Irritable Bowel Syndrome, please book a consultation with me to discuss your options. I have worked with many people experiencing a range of digestive issues using a blend of nutritional medicine, supplements, stress management techniques and acupuncture to help them experience lasting relief. |
Top 75 Naturopath Blogs & Websites For Naturopathic DoctorsAuthorDr. Keila Roesner is a Naturopathic Doctor. When not treating patients she is also an enthusiastic barefoot-strolling, music-loving, yoga-doing kitchen wiz - who also happens to be a wrestling fan. Categories
All
|
Let us take you from hormonal to whole.
|
Dr. Keila Roesner, BHSc ND
Naturopathic Doctor, Hormone Warrior and Your Wellness Cheerleader 247 Church Street, Stratford ON N5A 2R7 (519) 273-0900 [email protected] |
|









 RSS Feed
RSS Feed